Evaluating COVID-19 Control Measures
This post is based on a presentation moderated by Fred Boelter and given by Frank Pagone, Jacob Persky, and Benjamin Heckman. It is the sixth in the “Essentials of Pandemic Response” series based on AIHA's recently published ebook. The mention of specific products or companies does not constitute endorsement by AIHA.
At AIHce EXP 2021, Fred Boelter, CIH, PE, BCEE, FAIHA, moderated and introduced the educational session “An Evaluation of Ventilation Engineering Controls and Surface Cleaning Techniques on COVID-19 Risk Reduction Measures,” which provided updates on a topic discussed at AIHce the previous year. In March 2020—early in the pandemic—Boelter had written an essay about SARS-CoV-2 airborne transmission and the potential scale of the public health implications. He posted this essay to Catalyst, AIHA’s online member community. Over the coming months, Boelter and his colleagues collaborated on finding ways their occupational and environmental health and safety (OEHS) skillset could address COVID-19 in the workplace.
“As the data came in, it was increasingly recognized that simple techniques—masks, physical distancing, washing hands—do work effectively in meeting the source-pathway-receptor model,” said Boelter. (The source-pathway-receptor model is a framework for infectious disease controls that will be discussed completely in a coming blog.) “But humans spend upwards of 90 percent of their days inside a vehicle, residence, office, or facility,” he continued. “How that inside space is ventilated must be addressed, characterized, controlled, and certified.”
COVID-19 can be prevented by applying the traditional OEHS hierarchy of controls. However, “the challenge is in proving efficacy to a wary and weary public,” said Boelter.
Furthermore, ventilation systems are not simple, and there is not a single fix-all solution that OEHS professionals can tell their clients or members of the public to implement. In fact, it is unlikely that only one control will be enough to prevent COVID-19 transmission. A “Swiss cheese model” of layered controls is more likely to be effective.
Following Boelter’s introduction, industrial hygienists associated with environmental and occupational consulting firm RHP Risk Management then spoke on the findings of studies they had conducted on ventilation during the pandemic.
Evaluating COVID-19 Administrative Controls
Frank Pagone, PhD, CIH, spoke on cleaning and disinfection procedures as administrative controls for COVID-19. Although fomite transmission (occurring via contact with contaminated surfaces) of SARS-CoV-2 is not the predominant mode of transmission, it is still possible. Enhanced cleaning and disinfection procedures can prevent it.
“With the rapidly evolving state of knowledge,” said Pagone, “understanding and communicating the efficiency of various cleaning procedures is vital to risk communication, addressing fears, reducing confusion, and reducing the spread of disease.”
While related, cleaning and disinfection are not the same thing. “Cleaning” refers to the removal of dirt and contaminants such as germs from surfaces, while “disinfecting” refers to the use of chemicals to kill germs. While coronaviruses on surfaces naturally die within a few hours or days, especially in sunlight and warmer temperatures, killing the germs that remain on a surface after cleaning reduces disease transmission.
CDC recommends developing, implementing, maintaining, and revising a cleaning and disinfecting plan. This plan should cover what needs to be cleaned, how areas will be disinfected, and the resources needed, including personal protective equipment and EPA-approved disinfectants. The people responsible for cleaning and disinfecting must receive proper training, such as in proper use of PPE and correct handwashing, to avoid the transfer of germs and exposure.
To assess the efficiency of cleaning routines, RHP conducted three simulated sneeze scenarios under controlled conditions at their Exposure Science Laboratory. Each simulated sneeze scenario was followed by a different cleaning routine. The simulated “sneeze” liquid contained a fluorescent dye and a surrogate pathogen to help the researchers determine whether any of the “sneeze” remained in the room after cleaning and disinfection. After the “sneeze,” the room was cleaned following one of three procedures: cleaning by one occupant after the others left the room, routine cleaning by a janitor after all occupants left the room, and remediation by a COVID-19 cleaning professional. Eight high-touch locations around the room were assessed before and after the cleaning routine by application of ultraviolet (UV) light to detect the fluorescent dye, adenosine triphosphate (ATP) testing, and bacteria sampling. The cleaning personnel were not made aware of the sampling locations prior to cleaning.
ATP bioluminescence is an indirect measurement of the amount of living or dead organic residue on a surface, commonly used when assessing the cleanliness of food preparation surfaces. In contact with a swab reagent, ATP causes a light-producing chemical reaction. However, ATP surface testing does not measure viruses, including SARS-CoV-2, which cannot generate or store energy in the form of ATP. The surrogate pathogen used in the simulated sneeze was detectable by ATP testing, and, to assess the efficiency of disinfection, RHP researchers also sampled for the surrogate pathogen bacteria.
For each scenario, fluorescent dye from the simulated sneeze was visible on several surfaces throughout the room before, and sometimes after, the cleaning procedure. The most significantly affected surfaces included the desks, floor, doorknob, and whiteboard, as well as occupants’ hands.
ATP swab and surrogate pathogen samples were also collected before and after cleaning at each of the eight predetermined sampling locations. ATP testing results indicated that the janitorial company cleaned the most efficiently, as sampling showed an 80 percent reduction in ATP after their procedure. Cleaning by a room occupant and by a hired COVID-19 cleaning professional resulted in 45 and 68 percent reductions in ATP, respectively.
Sampling for the surrogate pathogen, however, showed that the hired COVID-19 cleaning professional reduced surrogate pathogen levels to below the threshold for detection. The surrogate pathogen was detected at sampling locations after cleaning by the janitorial staff and the room occupant.
To understand “normal” bacteria levels, ATP samples were also collected from uncleaned surfaces in various work settings, including those outside the simulation room. Many samples also showed elevated levels of ATP, indicating that these surfaces hosted a considerable amount of bacteria under “normal” conditions.
According to Pagone, the results of RHP’s study demonstrate the need to develop cleaning and disinfection procedures after first setting a “clean” control value by conducting ATP testing before and after cleaning. “Overall, it can be concluded that the cleaning scenario chosen influenced the effectiveness of removing or inhibiting the visual load and pathogen concentration as compared to the background levels,” said Pagone, “and the results support the importance of developing and understanding the goal of a site-specific cleaning and disinfecting plan.”
This study also demonstrated the distinction between cleaning and disinfecting, through comparing the janitorial company’s higher cleaning efficiency to the greater reduction in simulated pathogen concentrations by the COVID-19 cleaning professional that used a disinfectant fog. ATP testing may help determine whether chosen disinfectants are successful at killing certain contaminants.
Evaluating COVID-19 Engineering Controls
Jacob Persky, MPH, CIH, is another industrial hygienist with RHP. Recently, he has focused on engineering controls for COVID-19 to help facilities return to work. He spoke on work that RHP has done to characterize and measure risk related to aerosol and airborne transmission. While direct and indirect contact transmission through droplets traveling less than 6 feet is still recognized as the predominant form of SARS-CoV-2 transmission, as the pandemic unfolded, the virus’s ability to be spread over distances greater than 6 feet became better understood. Research at RHP has aimed to measure the degree to which a building ventilation system can control airborne transmission.
“To reduce risk, bring in more clean air,” said Persky, summarizing AIHA’s Reducing the Risk of COVID-19 Using Engineering Controls guidance document (PDF). “Clean air can come through one of two mechanisms: outside air or filtered, recirculated indoor air.”
In many climates, it isn’t feasible to completely rely on outside air. ASHRAE’s Building Readiness Guide (PDF) cautions that although the contribution of outside air should be maximized, it must remain within the capabilities of the HVAC system to maintain occupant comfort and allow the system to appropriately regulate humidity. The HVAC system should not bring in so much outdoor air that the building reaches dewpoint conditions, creating condensation and the potential for mold growth. As a result, most building ventilation systems will need to make use of recirculated air. This air will need to be cleaned of contaminants.
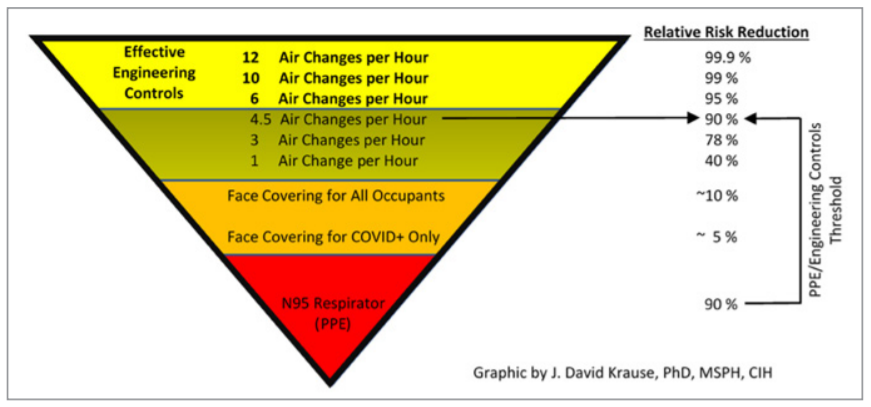
AIHA’s guidance document on engineering controls provides a table (Figure 1) that lists the level of protection or risk reduction afforded by different control measures, allowing for easy comparison. Persky noted that this table is particularly helpful for communicating risk to building owners and describing the benefits provided by different controls. According to this table, for instance, providing an air delivery rate of 4.5 changes per hour achieves a 90 percent reduction in risk, as does the use of N95 respirators by all building occupants. Theoretically, achieving a level of risk reduction greater than universal occupant respirator use is as simple as increasing the air delivery rate to six air changes per hour.
But it’s not always simple to determine the actual rates of air delivery and contaminant removal for every room in a building. Desktop calculations will often produce results different from the effective air change rate because buildings don’t have perfect air mixing conditions. One common, practical way of measuring the effective air change rate is through use of a tracer gas, as briefly discussed in the previous Essentials blog post, but there are alternative methods. A study produced through collaboration between the U.S. Transportation Command (TRANSCOM) and United Airlines used microsphere beads with diameters of 1–3 micrometers to assess ventilation in an airline cabin environment. The microsphere beads acted as a “challenge agent,” a surrogate for viral particles.
Studies like the one conducted by TRANSCOM require knowing the particle size of interest to test the ventilation system’s efficiency at removing those particles. A “free” SARS-CoV-2 virus particle is about 0.1 μm in diameter, but viruses are more often contained in droplets of 1–3 μm in diameter produced by coughing or sneezing; the TRANSCOM study used a challenge agent in that size range.
But it is also important to select a challenge agent that has physical and chemical properties closely resembling the particles of concern. Consequently, RHP selected a “DNA-tagged” aerosol challenge agent, veriDART by SafeTraces, a new building diagnostic tool that uses novel sequences of non-biological coding DNA in an aerosol spray released into an occupant space. Common OEHS equipment such as an air pump and filter cassette can be used to take air samples throughout a building, which are analyzed using quantitative polymerase chain reaction (qPCR) testing to determine the amount of novel DNA-tagged aerosol at various distances from the point source. This can be used to measure aerosol mobility and dispersion and the ventilation system’s air mixing characteristics. The RHP team compared the performance of the DNA aerosol method to tracer gas and particle count methods.
RHP evaluated various configurations of a replica classroom environment with ventilation rates ranging from 0.8–8 air changes per hour, comparing effective air change measurements with theoretical values. To summarize RHP’s findings, the tracer gas and particle count methods yielded air change rate measurements close to, but different from, the theoretical values. For example, for a theoretical value of 6 air changes per hour, RHP measured effective air change rates of 5 and 5.5 air changes per hour, respectively, using the tracer gas and particle count methods. Using the DNA-tagged aerosol method, however, different air change rates were recorded when sampling for different particle sizes because larger particles settled out of the air much more quickly than the smaller particles. The measured effective air change rate varies depending on the particle size fraction being measured.
“The main takeaway here,” said Persky, “is that tracer gas does not always necessarily align with the removal rate as measured, nor do each of these particle size fractions.” Decay rates—the rate at which particles fall out of the air due to gravity—are different for gases and aerosols. Therefore, while calculated air change rate values may overestimate risk reduction, air change rates based on measurements using tracer gases may also underestimate the contribution of dilution ventilation to risk reduction. RHP’s study used measurements taken with a DNA-tagged aerosol to characterize the magnitude of the difference between removal rates for aerosol particles of a size relevant to SARS-CoV-2 compared to a tracer gas. Future work, as of AIHce EXP 2021, included evaluating DNA-tagged aerosol measuring methods under more realistic conditions. An expanded version of this pilot study assessed the effect of filtration.
A stepwise process for introducing ventilation controls into a building is provided in the previous Essentials blog post.
Key Findings Concerning COVID-19 Controls
Benjamin Heckman, MPH, CIH, the former past chair of AIHA’s Risk Assessment Committee, then summarized the evolution of knowledge on COVID-19 and the development of COVID-19 information, controls, and risk assessment tools such as those discussed by Pagone and Persky. Significantly, the importance of aerosol transmission was not as well understood in March 2020 as it would be one year later.
The joint consensus statement on SARS-CoV-2 aerosol transmission (PDF) cosigned by AIHA and other scientific organizations in April 2021 addressed the way that understanding had changed up to that point and called on CDC and state health departments to account for aerosol and airborne transmission in their occupational health and respiratory protection programs. While none of the previously discussed modes of transmission (contact, droplet, airborne, and aerosol) should be ruled out, the joint consensus statement does highlight that inhalation seems to be more important than the initial risk attributed to contact transmission. Among other things, the joint consensus statement also advocates for the completion of an infectious disease standard applicable across all industries, the provision of federal funding for programs that prioritize the top of the hierarchy of controls, and the development of effective, simple, and inexpensive ventilation assessment tools. One of these tools was discussed in Persky’s presentation.
In preventing transmission via inhalation, ventilation is an important engineering control. However, controls can be layered upon each other to further reduce risk. While the risk of fomite transmission may be relatively low, the administrative controls highlighted by Pagone are also important and can work in conjunction with the implementation of ventilation controls.
Heckman concluded that, in order to control COVID-19 in the workplace, OEHS professionals must be able to use different techniques to assess and control risk as scientific understanding evolves. Control measures need to be tested, verified, and validated, such as through the methods described in this post, and their effectiveness documented. At this point in the pandemic, ensuring good ventilation system performance is particularly critical, and using DNA-tagged aerosol challenge agents may be a critical new way to do so.
Resources
AIHA: Effective and Safe Practices, Guidance for Custodians, Cleaning, and Maintenance Staff (PDF, Aug. 21, 2020)
AIHA: Employers’ Guide to COVID Cleaning and Disinfection in Non-Healthcare Workplaces (PDF, Aug. 11, 2020).
ASTM International: ASTM E741-11, Standard Test Method for Determining Air Change in a Single Zone by Means of a Tracer Gas Dilution (2017).
Boelter, Fred; Pagone, Frank; Persky, Jacob; and Heckman, Benjamin: “An Evaluation of Ventilation Engineering Controls and Surface Cleaning Techniques on COVID-19 Risk Reduction Measures,” AIHce EXP Virtual Conference Presentation (May 26, 2021).
The Journal of Hospital Infection: “Dismantling Myths on the Airborne Transmission of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2)” (April 2021).
Proceedings of the National Academy of Sciences: “A Guideline to Limit Indoor Airborne Transmission of COVID-19” (April 27, 2021).
United States Transportation Command and Air Mobility Command: “TRANSCOM/AMC Commercial Aircraft Cabin Aerosol Dispersion Test” (PDF, 2020).

Comments
There are no submissions.